Migraine is more than just a bad headache. According to the World Health Organization, it is one of the most prevalent and disabling medical conditions worldwide, affecting over 1 billion people. In the US alone, over 37 million people suffer from migraine, reports the American Migraine Foundation. Characterized by moderate to severe throbbing head pain and physical symptoms like nausea and light sensitivity, migraine attacks can be completely debilitating.

But a migraine episode is often foreshadowed by subtle changes in mood, cognition, and physical state known as “prodrome” symptoms. Recognizing these early warning signs is key to preventing attacks before the pounding headache phase kicks in. This article explores common prodrome symptoms, tips for identifying personal triggers, and lifestyle changes and treatments to manage symptoms and reduce migraine frequency.
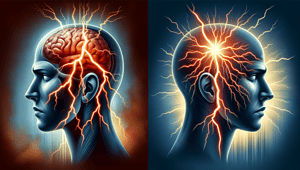
Phases of a Migraine Attack
Migraine attacks unfold in four distinct yet overlapping phases, explains the National Headache Foundation:
- Prodrome: Early subtle changes that warn an attack is brewing
- Aura: Visual, sensory or motor disruptions signaling the attack is imminent
- Headache: Throbbing head pain along with physical symptoms
- Postdrome: The after phase – fatigue, mental fogginess, mood changes
The prodrome phase, starting hours to days before head pain sets in, represents a critical window for aborting the oncoming attack. Heeding prodromal cues allows for early intervention to prevent full-blow migraine episodes.
Defining Prodrome Symptoms
Prodrome symptoms reflect the brain’s excitability before migraine pain starts, describes the Migraine Trust. While highly variable between attacks and individuals, they typically appear 12 to 48 hours pre-headache, states the American Headache Society.
Prodrome should not be confused with aura, despite some overlap. As the American Migraine Foundation explains, auras are acute neurologic events directly tied to migraine activation while prodromes manifest more gradually as subtle changes. Those who experience aura tend to always have the same manifestations with each attack.
Recurring Prodrome Patterns
Though prodrome symptoms differ widely, several stand out as most prevalent, reports the Cleveland Clinic:
- Mood changes: Irritability, depression, euphoria
- Food cravings: Strong desire for particular foods
- Neck stiffness: Shoulder and neck soreness
- Cognitive changes: Mental fuzziness, difficulty concentrating
- Sensory sensitivity: Increased sensitivity to light, sound, or smells
- Physical changes: Fatigue, nausea, frequent yawning or sighing
“Many patients experience these symptoms repeatedly before their attacks,” confirms the American Migraine Foundation. Recognizing individual patterns makes it easier to identify oncoming episodes.
Additional symptoms like dizziness, constipation, diarrhea or increased urination may emerge for some during prodrome, notes the Mayo Clinic.
Self-Monitoring Strategies
Pinpointing personal prodrome patterns requires diligent self-observation over multiple migraine cycles. Headache specialists propose various monitoring techniques:
- Keep a symptom diary: Record frequency, timing and specifics of symptoms before, during and after attacks. Tracking patterns helps identify triggers.
- Use a migraine tracking app: Migraine Buddy, Curelator and Headache Guru allow you to log symptoms, treatments and suspected triggers. Many generate reports to share with your doctor.
- Take quick notes: Jot down prodromal cues as soon as you notice them in a dedicated notebook or on your phone. Look back for emerging patterns.
“Even if you don’t feel the headaches yet, you’ll start to be able to tell when one is on the way based on how you’re feeling,” says the American Migraine Foundation. Reviewing records with a doctor can confirm suspicions and lead to better treatment.
Managing Prodrome Symptoms
Catching prodrome early opens the door to abortive therapy and preventive lifestyle changes, decreasing migraine frequency and disability, notes the National Headache Foundation.
- Stress management through yoga, meditation, therapy and relaxation is key as stress commonly triggers attacks.
- Good sleep habits since insufficient or inconsistent sleep can set off episodes.
- Regular mild exercise improves stress tolerance and neurochemical balance.
- Healthy eating and hydration to avoid blood sugar spikes and maintain electrolyte levels.
“Avoiding potential triggers is an integral part of migraine self-management,” emphasizes the Mayo Clinic. Keeping a headache diary helps pinpoint individual triggers like hormonal fluctuations, fasting, weather changes or particular foods. Successfully avoiding triggers is linked with substantial attack reduction for many patients.
Preventive and Abortive Medications
For frequent or severe migraine, prescription meds can significantly cut attack incidence. Commonly used types include:
Preventive medications: Taken daily, these medications dampen nerve transmissions to raise the migraine threshold. Beta blockers, antidepressants and anticonvulsants like topiramate have statistically proven preventive effects.
Abortive medications: Taken at prodrome onset, these aim to stop migraine in its tracks before the headache phase. Triptans are the gold standard – safe and effective for most when taken early. Other options include NSAIDs like ibuprofen or acetaminophen and newer gepants like Nurtec ODT.
Finding the right abortive therapy or preventive regimen takes some trial and error under medical guidance. Keeping a detailed headache diary speeds the process by elucidating effectiveness. Non-drug approaches like acupuncture, biofeedback or supplements may also help dial down attacks.
Start Spotting Those Early Cues
As a complex neurological disorder, migraine treatment takes a multi-pronged approach. But recognizing subtle prodrome patterns and heading off attacks before they gain steam provides real hope for sufferers. Self-monitoring, trigger avoidance and prompt intervention are key weapons in the battle against migraine.
References
- World Health Organization. (2023, April 13). Migraine. https://platform.who.int/mortality/themes/theme-details/topics/indicator-groups/indicator-group-details/MDB/migraine
- American Migraine Foundation. (n.d.). Migraine: About Migraine. https://americanmigrainefoundation.org/
- Mayo Clinic. (2023, November 14). Migraine headache. https://www.mayoclinichealthsystem.org/hometown-health/speaking-of-health/what-are-the-stages-of-a-migraine
- National Headache Foundation. (n.d.). The 4 Stages of a Migraine. https://www.stanmathewmd.com/blog/the-4-stages-of-a-migraine
- American Migraine Foundation. (n.d.). Migraine Signs & Symptoms. https://americanmigrainefoundation.org/migraine-signs-symptoms/
- Migraine Trust. (n.d.). Prodrome: Spotting the first signs of a migraine attack. https://americanmigrainefoundation.org/resource-library/migraine-prodrome-symptoms-prevention/
- American Headache Society. (n.d.). Migraine with Aura. https://americanheadachesociety.org/topic/migraine-with-aura/
- Cleveland Clinic. (n.d.). Migraine Prodrome Symptoms and Prevention. https://americanmigrainefoundation.org/resource-library/migraine-prodrome-symptoms-prevention/
- Boston Clinical Trials. (2022, April 18). 4 Subtle Signs of Migraines You Should Know About. https://www.primarycarewalkinmedicalclinic.com/
- American Migraine Foundation. (n.d.). Migraine Resource Library: Migraine Prodrome Symptoms and Prevention. https://americanmigrainefoundation.org/resource-library/migraine-prodrome-symptoms-prevention/