Migraines are severe, recurring headaches that affect over 37 million Americans. They can be debilitating and greatly impact one’s quality of life. Many people may experience their first migraine during adolescence or young adulthood, while others may suddenly develop migraines later in life. If you have recently begun experiencing migraines, you may be wondering – why now? Understanding the common causes of new onset migraines can provide valuable insight.
Migraines are different from regular tension headaches in their severity, symptoms, and underlying mechanisms. The main symptom is an intense throbbing headache, usually isolated to one side of the head. Migraine attacks can last anywhere from 4 to 72 hours. Many people also experience nausea, vomiting, sensitivity to light and sound, blurred vision, tingling sensations, and aura symptoms like seeing flashing lights.
The exact causes of migraines are not fully understood, but they seem to involve both vascular and neurological changes. Alterations in brain chemicals like serotonin as well as dilation and constriction of blood vessels play a role. There also appears to be a genetic component, with migraines running in families. Certain triggers can set off the biological cascade that leads to a migraine attack.
Common Causes of New Onset Migraines
There are a variety of factors that may explain the new development of migraine headaches in a person. Here are some of the most common causes:
Hormonal Fluctuations
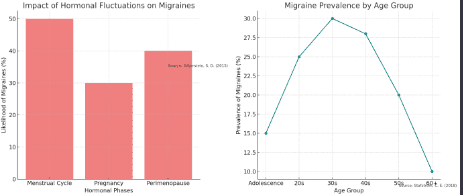
Hormonal changes are a very common migraine trigger in women. Fluctuating estrogen levels during the menstrual cycle can precipitate migraines in over 50% of female migraineurs. The days right before, during, or after a period are when migraines are most likely to occur.
Pregnancy is another time when female sex hormones rise and fall dramatically. Migraines often improve during the second and third trimesters when hormone levels are high and steady. However, they frequently recur during the postpartum period.
Perimenopause – the transition to menopause – is also marked by hormonal ups and downs. This can lead to new onset migraines in some women. Declining estrogen is thought to play a role.
Stress
Stress is one of the most commonly self-reported migraine triggers. Stress activates the sympathetic nervous system and leads to the release of hormones like cortisol. This stress response can initiate the neurochemical events that culminate in a migraine attack.
Starting a new job, financial pressures, relationships issues, major life changes, trauma, and even positive excitement can induce migraines in stress-prone individuals. Managing stress through relaxation techniques, massage, meditation, exercising, and getting enough sleep may help prevent stress-induced migraines.
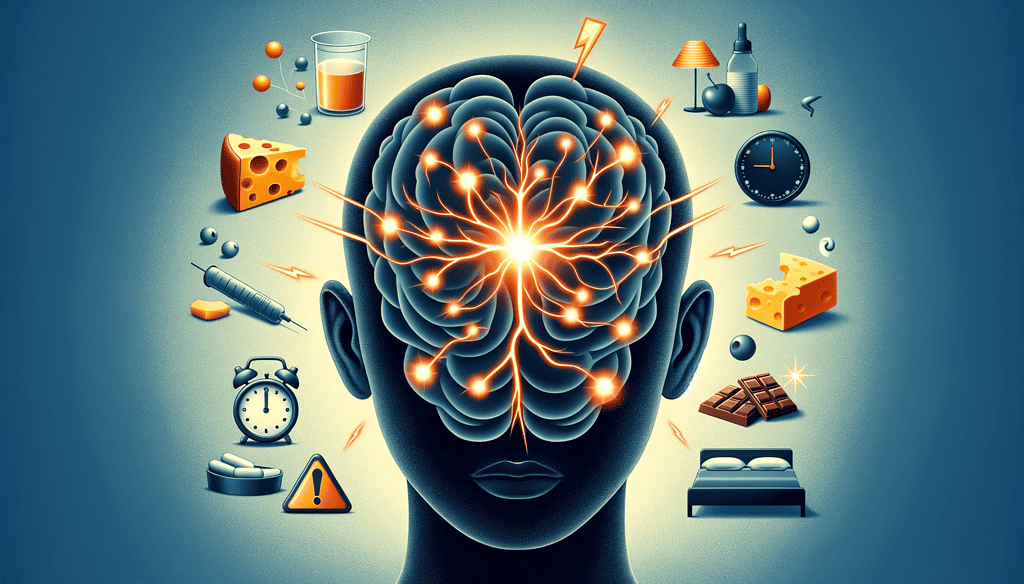
Dietary Factors
Certain foods, drinks, and eating patterns can activate migraines. Common dietary migraine triggers include:
- Aged cheeses like cheddar, Parmesan, feta
- Processed meats with preservatives like nitrates
- Chocolate
- Alcohol, especially red wine
- Caffeine (can be a trigger if consumed irregularly)
- Artificial sweeteners like aspartame
- Fasting or skipping meals
If you have recently made major changes in your diet, pay attention to whether any new foods or drinks precede your migraine attacks. An elimination diet can help identify your personal migraine triggers.
Sleep Disturbances
Lack of quality sleep is another major contributor to migraine onset. Not getting enough sleep or having inconsistent sleep times can reduce the brain’s threshold for headaches. Sleep deprivation and even weekend “catch up” sleep have both been linked to an increase in migraine days for suffers.
Conditions like sleep apnea, restless leg syndrome, and insomnia disrupt sleep. Getting adequate nightly rest, sticking to a schedule, and treating any underlying sleep disorders can help diminish migraines.
Environmental Factors
Bright or flickering lights, loud noises, strong odors – sensory stimuli like these can trigger migraines in susceptible people. This may be due to their effects on brain pathways involved in migraine pathogenesis. Cigarette smoke, perfumes, cleaning products with strong fumes, and environmental allergens can all set off migraines.
If you start a new job with fluorescent office lighting or move to a neighborhood with different scents and smells, be aware of possible links with your migraine start. Wearing sunglasses, using noise-canceling headphones, and avoiding triggers can help relieve environmental migraine triggers.
Medications
Certain prescription and over-the-counter medications may cause medication-overuse headaches. Some medications themselves directly act as migraine triggers. Common culprits include:
- Overusing NSAIDS like ibuprofen and naproxen sodium
- Triptans like sumatriptan
- Opioid pain medications
- Birth control pills, especially those with estrogen
- Certain antidepressants
- Asthma and heart medications like beta blockers
If your migraines started after beginning a new medication, speak with your doctor about alternatives that are less likely to trigger migraines. Preventative medications may also help counteract migraines caused by other required medications.
Underlying Medical Conditions
In some cases, what presents as new onset migraines may be attributable to another underlying medical condition. These include:
- High blood pressure
- Head injuries or trauma
- Sinus infections
- Sleep apnea
- Head and neck tumors
Severe headaches accompanied by other neurologic symptoms, mental status changes, vision loss, or head injury could indicate a secondary cause. Seeking timely medical evaluation is recommended for new onset migraines to rule out concerning underlying conditions.
When to Consult a Doctor
It is important to see a doctor if you are experiencing new migraines, especially if they are frequent and severe. A primary care physician can check for underlying conditions and medication side effects that may be contributing to migraines. They may recommend you see a neurologist or headache specialist for further diagnosis and treatment.
These migraine specialists can help distinguish between migraine and other headache types. They can order imaging or blood work to rule out secondary causes. If your migraines are indeed primary, they can recommend medications and lifestyle changes to prevent and treat your migraine attacks. Don’t resign yourself to living with debilitating new onset migraines – consult a doctor to find relief.
Conclusion
New onset migraines can be concerning but getting to the bottom of the cause is the first step. Hormonal shifts, dietary triggers, sleep issues, stress, medications, and medical conditions are common culprits. Seeing a doctor for an evaluation can identify or rule out major causes, while tracking headache triggers on your own can provide additional insight. Understanding why you may suddenly be getting migraines empowers you to take action to prevent future attacks.
References
- Buse DC, Reed ML, Fanning KM, Bostic R, Dodick DW, Schwedt TJ, Lipton RB. Comorbid and co-occurring conditions in migraine and associated risk of increasing headache pain intensity and headache frequency: results of the migraine in America symptoms and treatment (MAST) study. The journal of headache and pain. 2020 Dec;21(1):1-2.
- Martin PR. Managing headache triggers: think ‘coping’ for improved outcomes. The journal of headache and pain. 2007 Jun 1;8(3):174.
- Silberstein, S. D. (2015). Menstrual migraine. Cephalalgia, 35(4), 328–331. https://doi.org/10.1177/0333102414564892
- Smitherman, T. A., & Maizels, M. (2020). Headache during pregnancy and postpartum. Neurologic Clinics, 38(3), 527–540. https://doi.org/10.1016/j.ncl.2020.04.001
- Stafstrom, C. E. (2018). Migraine biology and models of migraine biomarkers. Headache. https://doi.org/10.1111/head.13387
- Worthington, I., Pringsheim, T., Gawel, M. J., Gladstone, J., Cooper, P., Dilli, E., Aube, M., Leroux, E., Becker, W.J. (2013). Canadian Headache Society Guideline: acute drug therapy for migraine headache. The Canadian journal of neurological sciences. Le journal canadien des sciences neurologiques, 40 Suppl 3(Suppl 3), S1–S80.
- Bar Chart – Impact of Hormonal Fluctuations on Migraines: This chart depicts how hormonal changes, particularly in women during phases like the menstrual cycle, pregnancy, and perimenopause, influence the likelihood of experiencing migraines. The citation “Source: Silberstein, S. D. (2015)” provides the reference for this data.
- Line Graph – Migraine Prevalence by Age Group: This graph shows the prevalence of migraines across different age groups, from adolescence to 60 and beyond. It illustrates the trends in migraine prevalence at various life stages. The citation “Source: Stafstrom, C. E. (2018)” is included to reference the source of this information.